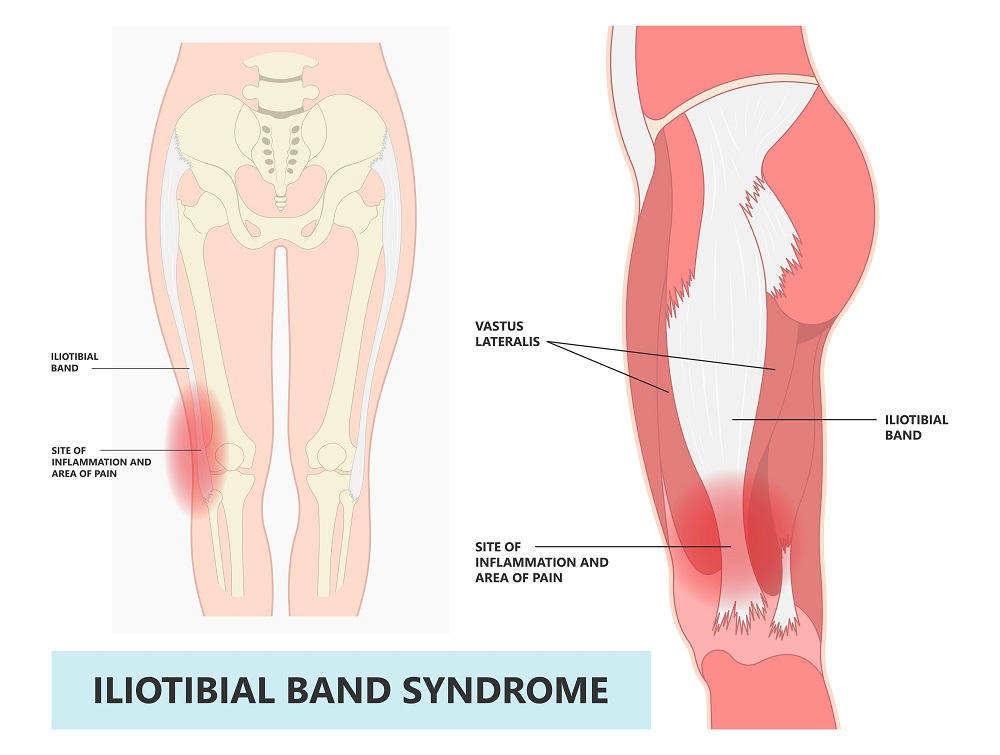
If you’re a runner, you might have heard of IT band syndrome (ITBS), a common injury that accounts for one tenth of all running injuries1. It is the second most common injury for runners.1 The IT band is a thick band of connective tissue that runs along the outside of the thigh, from the hip to the knee. It is characterized by pain and inflammation in the IT band, which can cause discomfort and limit your running performance. In this blog, we’ll take a closer look at IT band syndrome and why it affects runners.
What is IT band syndrome?
IT band syndrome is a common overuse injury that occurs when the IT band becomes irritated and inflamed. From a historical perspective ITBS is caused by excessive friction of the distal iliotibial band as it moves over the lateral femoral epicondyle during repetitive knee flexion and extension.2 The IT band is responsible for stabilizing the knee during running, and repetitive movements can cause the band to become overworked and inflamed. IT band syndrome is most commonly experienced by runners, but it can also affect other athletes, such as cyclists and hikers.
What are the symptoms of IT band syndrome?
Symptoms of IT band syndrome include pain and tenderness on the outside of the knee, especially during running or other activities that involve bending the knee. You may also experience a popping or snapping sensation in the knee, and the pain may worsen when running downhill.
What causes IT band syndrome in runners?
There are several factors that can contribute to the development of IT band syndrome in runners. Here are a few of the most common causes:
- Overuse and repetitive movements: Running involves repetitive movements of knee flexion and extension that can put stress on the IT band. If you’re running too much or too often, the IT band can become overworked and inflamed.
- Weak hip and glute muscles: The hip and glute muscles play a crucial role in stabilizing the pelvis and knee during running. If these muscles are weak, the IT band may be put in a biomechanical disadvantage causing friction of the distal portion of the IT band, leading to increased pain and inflammation.
- Biomechanical alterations: If you’re not using proper running form, you may be putting more stress on one side of the body, leading to imbalances and increased strain on the IT band.
- Reduced flexibility: Tight muscles, particularly the hip flexors, TFL, and glutes can contribute to the development of IT band syndrome. When these muscles are tight, they can pull on the IT band, leading to increased friction and inflammation.
How can IT band syndrome be treated and prevented?
If you’re experiencing symptoms of IT band syndrome, it’s important to take steps to address the underlying causes and prevent further injury. Here are a few strategies that can be effective:
- Reduce workload: If you notice at a certain time or mileage the pain occurs reduce your workload of running to a pain free zone. If pain is constant during run rest might be your best option to allow structures to heal.
- Mobility: Stretching can help to alleviate tightness in surrounding muscles around the IT band. Remember the IT band is connective tissue and not a muscle so the focus should be on the surrounding muscles.
- Strengthening exercises: Strengthening exercises can help to address imbalances and weakness in the hip and glute muscles. Focus should be on pain free exercises that target the hip abductors, extensors and all surrounding musculature.
- Foam rolling: Foam rolling can be an important tool to help increase your mobility. Foam rolling structures surrounding the IT band will help decrease tension on the lateral knee. Please avoid foam rolling the IT band because it is connective tissue and not a muscle.
- Running gait biomechanics screen: This might be a great time to get an evaluation from a running gait expert or physical therapist to determine if there are any alterations in biomechanics causing stress on your IT band.
- Gradual return to running: When you’re ready to return to running, it’s important to do so gradually. Start with short, easy runs and gradually increase the distance and intensity over time. There are some great return to run programs that will gradual build resilience over time.
IT band syndrome can be a debilitating injury and can prevent you from running pain free. If running is your passion, it’s important to be proactive and work on some strategies above to reduce the likelihood of IT band syndrome stopping your joy of running. If it’s in the early stages, applying a knee brace might be an option which helps decrease discomfort and allow you to continue running while you work on fixing the cause. Zamst offers the RK-1 Plus , an IT band knee brace which is specifically designed to reduce the strain on the outside of the knee. If running is important to you, Zamst provides you with the tools and bracing options to continue doing what you love to do.
If you need help with choosing the best knee brace, the Zamst Brace Finder can guide you in finding the best knee brace to accommodate your needs.

ABOUT THE AUTHOR
EVAN JEFFRIES is a physical therapist with a Doctorate in Physical Therapy (DPT) from the University of St. Augustine for Health Sciences. He is also the owner of Evolving Motion and has vast knowledge of the musculoskeletal system and has treated many orthopedic conditions by bringing a proactive approach to healthcare and lifestyle. Recently he has also been active on social media as an injury analyst mainly in related to injuries NBA players have sustained. Evan can be followed on his social media accounts.
- Aderem J, Louw Q. Biomechanical risk factors associated with iliotibial band syndrome in runners: a systematic review. Aderem and Louw BMC Musculoskeletal Disorders (2015) 16:356
- Khaund R. Iliotibial band syndrome: A common source of knee pain. Am Fam Physician. 2005;71:1473–5.






