![FullSizeRender[1]](https://blog.zamst.us/wp-content/uploads/2016/07/FullSizeRender1.jpg) Anatomy: The achilles tendon, also known
Anatomy: The achilles tendon, also known
as Calcaneal tendon, is the
culmination of three muscles before
their attachment on the calcaneus
(heel bone). The three muscles in
descending depth from the back of the
calf are gastrocnemius, plantaris, and
soleus. As a group they are sometimes
referred to as the triceps surae. The
muscles and tendon complex act to:
plantarflex the ankle (point your foot
and toes away from you), propel the
heel off the ground when contracting concentrically, and work eccentrically to control the progression and stabilize the tibia when in a trailing position during ambulation.
Epidemiology: Approximately 75% of rupture cases occur in the “vascular watershed” span of the 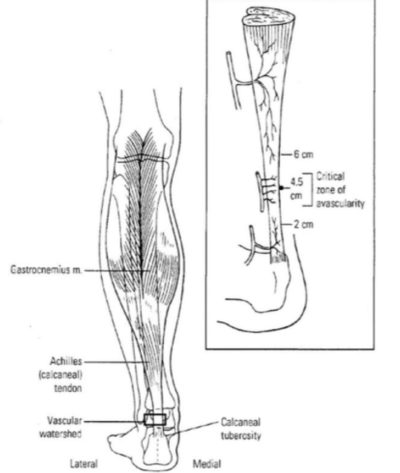
tendon around 2-6 cm proximal to the insertion on the calcaneus. Incidence rate of 18 cases per 100,000. 68% of ruptures occur during athletic activities. Occurrence is more common in men than women with the average age of injury similar at (43.8 and 55.1 years old respectively.
Causes:
● Often occurs during physical activity involving increase of load, duration, intensity, change in terrain or footwear.
● A forced dorsiflexion (landing after a jump, or driving/planting the foot into the ground) with simultaneous muscular contraction of the triceps surae produce the highest load on the tendon.
● Often longstanding degenerative changes and pain in the tendon precipitate rupture.
Clinical Presentation:
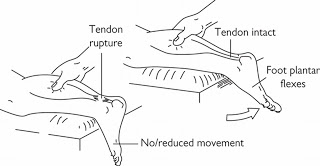
Flaccid calf musculature with divot and or loss of continuity of tendon.
Positive Thompson test (seen below)
Treatment options:
Return to full function can be achieved in
6 months, and full sport in 12 months.
● Non-surgical: Similar functional outcomes to surgery, and similar re-rupture rates and other risks.
● Surgical: Slightly faster recovery time. Quicker return to sport.
○ Open surgery: good strength to the repair, low re-rupture rates and reliably good
endurance and power after recovery.
○ Percutaneous surgery: Decreased rates of deep wound infection.Physical Therapy:
● Casting or walking boot for immobilization 6-12 weeks. (starting with heellift to offload tendon during first phases of healing)
● Early postoperative protective weight bearing
● Use of protective devices that allow for postoperative mobilization
● Research has shown that early mobilization has had a positive effect on thetendon healing process.
Prevention:
● Dose into activities.
● Utilize proper footwear
● Seek medical attention: Including physical therapy early in suspectedAchilles tendonitis or pathology to help maintain integrity of tendon.
● Brace: Zamst AT-1: Allows the Achilles tendon to glide in alignment andmaintain proper foot motion. The AT-1 will assist in pushing the foot down and reduce the tension on the Achilles tendon.
References:
Holm C, Kjaer M, Eliasson P. Achilles tendon rupture–treatment and complications: a systematic review. Scand J Med Sci Sports. 2015;25(1):e1-10.
Huang J, Wang C, Ma X, Wang X, Zhang C, Chen L. Rehabilitation regimen after surgical treatment of acute Achilles tendon ruptures: a systematic review with meta-analysis. Am J Sports Med. 2015;43(4):1008-16.
Pedowitz D, Kirwan G. Achilles tendon ruptures. Curr Rev Musculoskelet Med. 2013;6(4):285-93.
Saidoff DC, McDonough AL. Critical Pathways in Therapeutic Intervention: Extremities and Spine. St. Louis, Mosby Elsevier, 2002, pp.1043-59; 717; 832.
http://img.bleacherreport.net/img/article/media_slots/photos/001/098/399/VinceWilfork_crop_exact.j pg?w=650&h=433&q=85,http://images.slideplayer.com/14/4311406/slides/slide_53.jpg






